2025 Pharmacy Benefits-Prime Therapeutics
Effective January 1, 2025, Prime Therapeutics (Prime) is the pharmacy benefit manager for the Local Government Health Insurance Plan. To receive your medications at a retail pharmacy, please show your new combined medical/pharmacy Blue Cross and Blue Shield of Alabama member ID card at your pharmacy. Prime’s retail pharmacy network will include thousands of retail pharmacies – including national chains and most independent pharmacies.
Plan Design
| Tier | Type | Copay |
|---|---|---|
| Tier 1 | Generics |
Member pays a $15 copay or the full cost of the medication, whichever is less. |
|
Tier 2 & 3 |
Preferred & non-preferred brands | Member pays 100% of the cost of the drug at the point of sale and files for 80% reimbursement after $200 deductible has been met. |
| Tier 4 | Certain high-cost specialty drugs and brand-name diabetic drugs | Members are responsible for 20% coinsurance at the point of sale. The plan covers medications at 80%. |
| Specialty Medications | Found in Tiers 1-4 | Filled through designated specialty pharmacies, specialty medications can be found in multiple tiers and follow the benefit structure of that tier. |
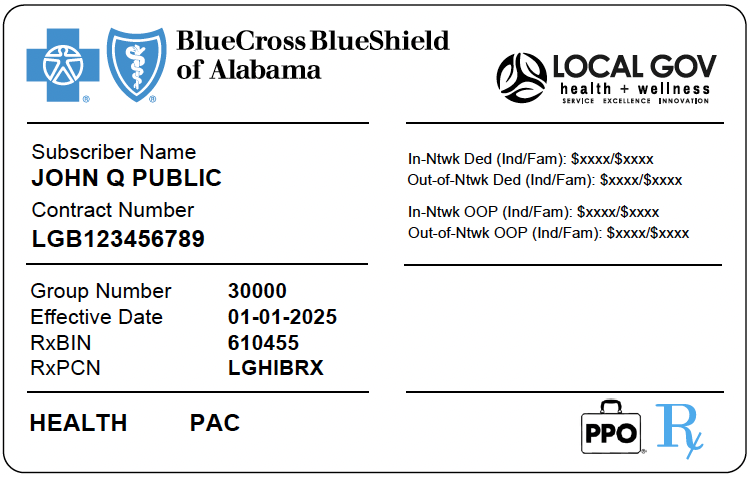
New Insurance Cards
All subscribers will receive new insurance cards in the mail in the coming weeks. The new combined medical/pharmacy Blue Cross and Blue Shield of Alabama member ID card can be used at both your provider's office and your pharmacy.
If you do not receive your new card by January 1, 2025, create an account at AlabamaBlue.com or download the Alabama Blue app for a virtual copy of your member ID card.
Below is an example of the new member ID card:
Contact Us
If you or your provider have questions about your pharmacy benefits, please call the customer service number on your member ID card (TTY: 711). This is the same customer service number as your medical benefits.
Blue Cross and Blue Shield of Alabama Member Services
800-321-4391 | Monday-Friday, 7am-6pm Central Time
After-hours pharmacy calls will be directed to Prime Therapeutics.
All benefits below regarding Prime Therapeutics are applicable and accessible beginning January 1, 2025.
Prime’s Member Portal
Beginning January 1, 2025, you can visit MyPrime.com to access helpful tools to:
- See your benefits and view prescription history
- Download forms
- Check the list of covered medicines
- Learn more about specialty pharmacy services
- Track prior authorizations
Direct Member Reimbursement
For name brand prescriptions, you will pay 100% out-of-pocket at the point-of-sale and then file for 80% reimbursement (subject to your $200 deductible) with Prime Therapeutics.
Note: Generic medications are not eligible for claim reimbursement.
Accredo Specialty Pharmacy
Your plan is committed to giving you a specialty pharmacy that offers the medicines and support you need to manage your complex health issues.
- Access to 98.1% of specialty medicines based on claims volume, which means you are likely to get all your specialty medicines from one specialty pharmacy
- Simple communication, including refill reminders, through phone, email, text or web, whichever you prefer
- A mobile app that allows you to track prescriptions, make payments and set reminders to take your medicines
- 500 condition-specific pharmacists and 600+ nurses, all offering one-on-one counseling
- Free standard delivery
- 24/7 support from Accredo Specialty Pharmacy at 833-715-0965.
If you currently take a specialty drug covered under our plan, you will receive a letter in the mail from Prime Therapeutics with instructions on how to create an online account and fill your medication.
FlexAccess Program
The FlexAccess program is designed to help you save money on certain specialty medications by obtaining copay assistance from drug manufacturers when available. Once you start receiving the manufacturer-funded copay assistance through the FlexAccess program, your copay will be between $0-$35 per eligible prescription. You will continue to pay the reduced copay amount until the end of the calendar year even if your copay assistance funds run out prior to December 31. While enrolled in the program, only your copay amount will apply toward your annual maximum out-of-pocket.
NOTE: Not all specialty medications are eligible for manufacturer copay assistance through the FlexAccess Program. For specialty medications that are not eligible through the FlexAccess program, members will pay their applicable drug tier cost share.
Call FlexAccess at 888-302-3618 to see if your medication(s) is on the list of eligible medication(s) for manufacturer assistance. If your medication is eligible, they will provide you with next steps to enroll with the manufacturer to obtain funding.
Prior Authorizations
Members with medications that require an updated prior authorization on or after January 1, 2025 will receive a letter in the mail explaining the approval process, the prior authorization expiration date, and what information you need to discuss your provider. If you or your provider have started the prior authorization process, no further action is needed.
2024 Pharmacy Benefits-OptumRX
The deadline to submit the Direct Member Reimbursement (DMR) by mail to OptumRX for eligible 2024 tier 2 and 3 prescription drugs is February 28, 2025.
OptumRx is the pharmacy benefit manager for members of the Local Government Health Insurance Plan. If you have questions about your OptumRx prescription drug coverage, please call 1-844-785-1603.
- 2024 OptumRx Benefit Booklet
- 2024 Prescription Drug Formulary
- ACA Preventative Care Medication List
- Specialty Pharmacy Medication List
Using tier 1 or preferred medications can help you pay your lowest out-of-pocket cost. Our health insurance plan has multiple tiers.
| Copay | Supply Limit | |
|---|---|---|
| Tier 1: Generics | $15 copay or the cost of the medication, whichever is less. |
Up to a 30-day supply Up to a 60-day supply after initial 30 day fill (maintenance medications) |
|
Tier 2: Preferred Drugs |
Member must pay 100% of the cost of the drug and file for 80% reimbursement after $200 deductible has been met. | Up to a 90-day supply |
| Tier 3: Non-Preferred Drugs | Member must pay 100% of the cost of the drug and file for 80% reimbursement after $200 deductible has been met. | Up to a 90-day supply |
| Tier 4 | For certain high-cost drugs, members are responsible for 20% coinsurance at the point-of-sale. Plan covers medication at 80% |
Days supply varied by medication Refer to the formulary booklet for covered medications |
Pharmacy at your fingertips
The OptumRX website and app gives you the information you need to make the most of your pharmacy benefit.
Visit the OptumRx member portal for easy access to:
- Manage all your prescriptions on a single dashboard
- Update your information and complete your health profile
- Compare prices at local pharmacies
- Find your lowest prescription cost
- Locate your pharmacy and get driving directions
- Keep track of your health history
- Learn more about your drugs
- Take it all with you through the mobile app
- Manage prescriptions for your dependents and family members, where appropriate.
Prescription Drug Reimbursement
For name-brand prescriptions, you will need to pay 100% out-of-pocket at the point-of-sale, then file for your 80% reimbursement (subject to your $200 deductible) with OptumRx. The deadline to submit the Direct Member Reimbursement (DMR) by mail to OptumRX for eligible 2024 tier 2 and 3 prescription drugs is February 28, 2025.
Note: Generic medications are not eligible for claim reimbursement.
Prior Authorizations
A prior authorization is an approval you or your doctor obtain before you can get coverage for certain medications. The review process helps make sure the medication you’re taking is appropriate and effective for your condition. Check the prescription drug list, also known as the formulary, to find out if a medication you take requires a prior authorization.
Specialty Pharmacy
Do you take a specialty medication? You can fill your specialty medications at OptumRX Specialty Pharmacy. Call 1-855-427-4682 or visit specialty.optumrx.com for more information.
OptumRx Drug Card
To view and print your OptumRx card, sign in to your OptumRx account through the mobile app or through the member portal.

